Cervical cancer is linked to Human Papillomavirus (HPV), which is a sexually transmitted infection that contributes to over 99% of all cases. Specifically, HPV high-risk types can transform normal cells into cancerous lesions, which makes regular screening a pivotal line of defense. According to the Centers for Disease Control and Prevention, most sexually active individuals will contract HPV at some point, albeit many infections clear spontaneously.
When we discuss Pap smear vs HPV test, it’s vital to note that these screenings commonly reveal infections that are caused by strains such as HPV 16. This is the most carcinogenic subtype that’s linked to cervical cancer. Additionally, certain diagnostic tests can identify HPV mRNA E6/E7 results, which imply active viral replication and a higher chance of cellular damage.
Because the virus can remain undetected for years, regular cervical exams are essential. Early detection of HPV high-risk types can dramatically reduce the risk of advanced cervical cancer.
For further insights on regular Pap smear check-ups, you can refer to Well-Woman Exams: Pap Smear & HPV Care on NOUL’s website.
HPV High-Risk Types and Their Links to Cancer
 Source : Wikimedia
Source : Wikimedia
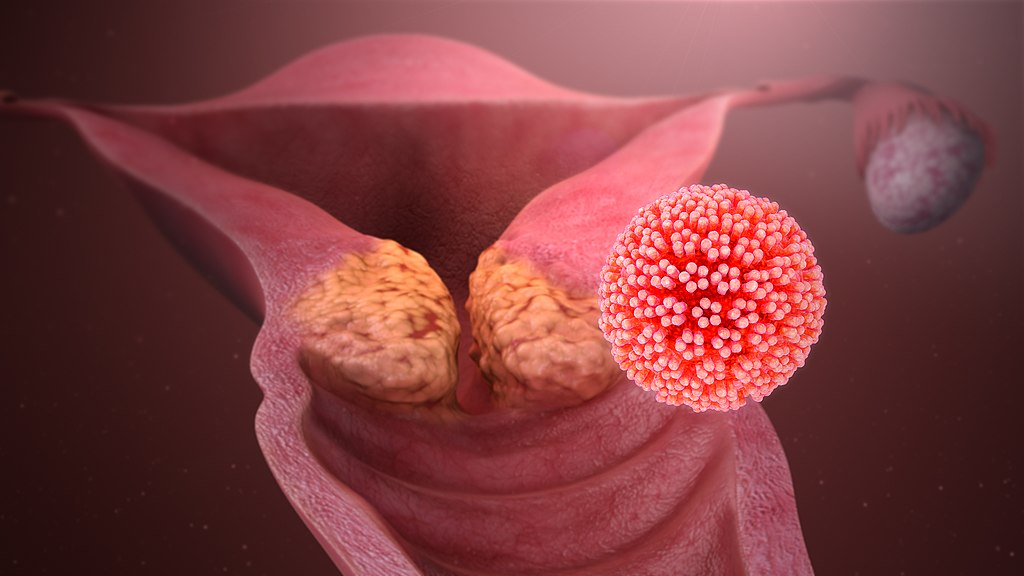
HPV comprises more than 100 unique strains. A smaller subset is responsible for the majority of cervical cancer cases. Among these, HPV 16 leads the pack. Studies consistently highlighted its strong correlation with both cervical and other cancers, including head and neck tumors.
HPV genotype 18/45, which belongs to the Alpha-7 HPV family, is frequently implicated in a more aggressive but less common cervical cancer form known as adenocarcinoma. When tests demonstrate HPV mRNA E6/E7 detected, it suggests that these high-risk strains are actively producing viral proteins (E6 and E7). These proteins can disable the cell’s natural defense mechanisms against tumor growth.
Although the immune system clears HPV infections, chronic infection with these HPV high-risk types significantly raises the risk of precancerous changes. According to the World Health Organization, up-to-date screening is vital since early intervention can halt disease progression.
Learn more about HPV strains by checking out the Female Reproductive System & Cervical Tests.
The following table highlights some high-risk strains:
Understanding HPV mRNA
 Source : Photosonic
Source : Photosonic
When the HPV infects cervical cells, it begins to produce viral messenger RNA (mRNA). The presence of HPV mRNA E6/E7 detected on a diagnostic test indicates that the virus is present and active.
E6 and E7 proteins can disable essential cell regulators that control DNA repair and programmed cell death. Among HPV high-risk strains, HPV 16, 18, 45 are particularly active in producing these proteins.
For more insights into visible symptoms that could accompany active HPV infections, see 3 Visible Signs of Cervical Cancer.
Pap Smear vs HPV Test: Screening Differences
 Source : Flickr
Source : Flickr
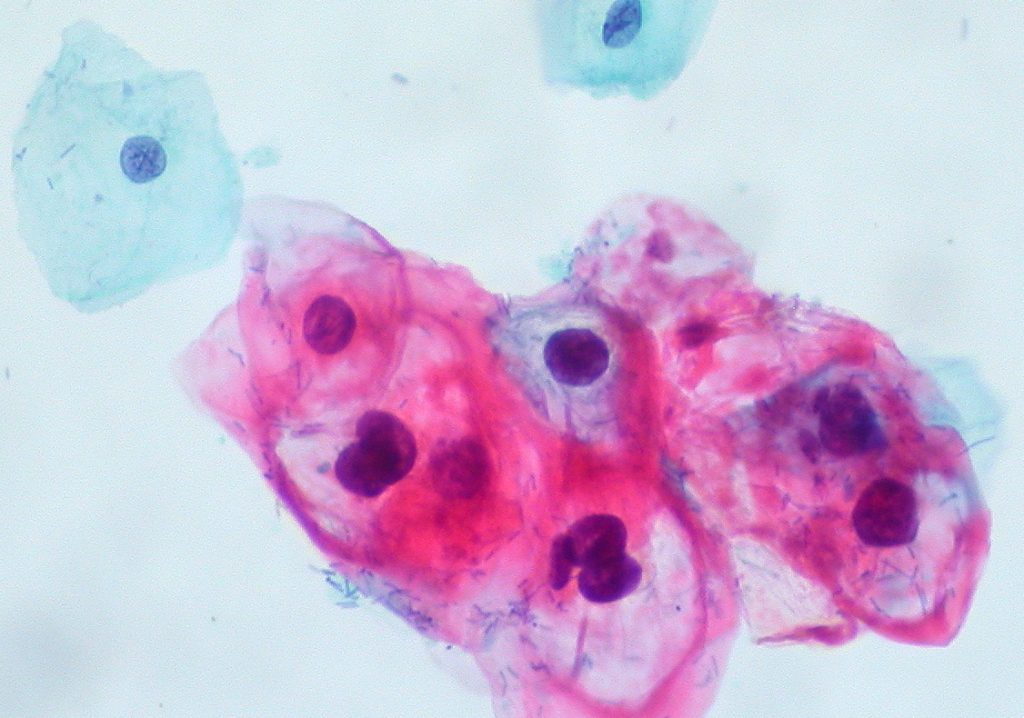
The debate over Pap smear vs HPV test revolves around which test provides a clearer picture of cervical health. A Pap smear (or Pap test) examines the cervix microscopically to identify cellular irregularities that might have already formed as a result of HPV high-risk types such as HPV 16 or HPV genotype 18/45.
Conversely, an HPV test targets the virus itself. So, it identifies the genetic material that’s associated with high-risk strains. This is especially useful for catching infections early. For instance, if an HPV test detects mRNA E6/E7, clinicians can confirm an active infection with potential for rapid progression.
Despite its strengths, relying solely on the HPV test may not be sufficient. It doesn’t clarify whether the infection has already induced cellular changes or the severity of any existing abnormalities. This is why the combination of both methods (i.e., co-testing) is highly recommended. Co-testing offers a more complete assessment, detecting HPV (particularly HPV 16) and identifying early cellular changes.
For an in-depth reading on Pap smear results (HSIL, LSIL, ASC-H, ASC-US, SCC, and NILM), visit NOUL’s post on HSIL, LSIL, ASC-H, ASC-US, SCC, and NILM.
NOUL’s miLab™ CER: A New Era in Cervical Cancer Diagnosis
 Source : NOUL
Source : NOUL
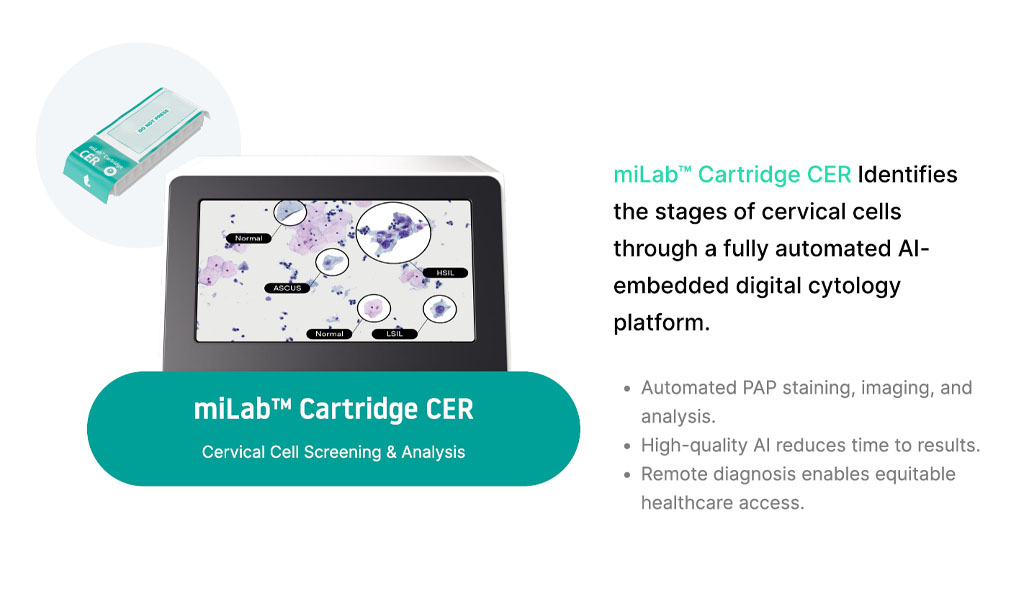
Despite the strengths of Pap smears and HPV tests, challenges remain. NOUL has introduced miLab™ CER, an innovative diagnostic solution that enhances cytological analysis using artificial intelligence. This platform examines cellular changes under the microscope, providing a precise cytological assessment that complements HPV test results for a more comprehensive diagnosis.
What sets miLab™ CER apart is its capacity to spotlight tiny morphological shifts that can be overlooked in standard screenings. By leveraging AI-driven analysis, miLab™ CER enhances the detection of cellular abnormalities that might indicate HPV-related changes, improving diagnostic accuracy.
If you want to learn more about how this tool can be integrated into existing screening programs, explore the detailed product features on NOUL’s miLab™ CER page.
Conclusion
 Source : Flickr
Source : Flickr
Cervical cancer is highly preventable, with early detection playing a crucial role in reducing risk. At its core, HPV 16 and other HPV high-risk types drive the disease process. Moreover, when an active infection is indicated by HPV mRNA E6/E7, rapid diagnostic follow-up can be lifesaving.
In this context, miLab™ CER enhances the diagnostic process by combining AI-driven technology with advanced cytological analysis. This approach not only provides early warnings but also delivers a precise assessment of cervical cellular changes, enabling more informed clinical decisions.
To learn more about how miLab™ CER can support your cervical screening program, visit our Product Inquiry page and get in touch with us today.