Malaria is a life-threatening disease spread from person to person by mosquitoes. However, the disease is not caused by the mosquito itself, but by a parasite it carries. All forms of malaria involve the Plasmodium family of parasites—the deadliest is Plasmodium falciparum, which accounts for over 95% of malaria cases and deaths in sub-Saharan Africa, according to recent WHO estimates.
Malaria detection efforts are slowly improving thanks to the growing use of rapid diagnostic tests (RDTs). Currently, microscopic examination of stained blood smears is the most reliable technique to determine parasite density and categorize its specific developmental stage—critical for effective treatment planning.
In this guide, we’ll walk through how to identify Plasmodium falciparum in blood smears, focusing on the key life stages: the distinctive falciparum ring form, trophozoite, schizont, and gametocytes.
Blood Smear Examination and Diagnostic Challenges

Source: Flickr
The diagnostic gold standard for confirming a malaria infection is light microscopy with Giemsa-stained blood smears. In simple terms, this procedure involves spreading a blood sample onto a slide, staining it, and then examining it under a microscope to identify the malaria parasite. While highly effective, the process is time-consuming and demands specialized expertise.
Thick blood smears increase the likelihood of detecting parasites due to the higher concentration of blood, making them ideal for initial diagnosis. Thin smears, on the other hand, provide clearer detail, allowing for accurate species identification and differentiation based on parasite morphology.
Microscopically, P. falciparum is notable for several features:
- Multiple ring forms within a single red blood cell.
- Accolé forms, where the ring appears attached to the edge of the RBC membrane.
- Banana-shaped gametocytes, which are morphologically unique to P. falciparum.
As mentioned, the main issue in sub-Saharan African healthcare settings is the lack of healthcare infrastructure. That extends to basics, like reliable electricity and laboratory infrastructures, to a shortage of trained microscopists. Even if this infrastructure is in place, a steady supply of quality reagents and other supplies is essential.
These severe limitations hamper or delay diagnoses or lead to misidentification. Such confusion often leads to delayed or incorrect treatment, worsening outcomes. Early intervention remains crucial.
Plasmodium falciparum in Blood Smears: Parasite Stage Overview
P. falciparum undergoes several stages during its lifecycle. These stages can take place in mosquitoes or humans. Below, we cover the stages relevant to malaria diagnosis.
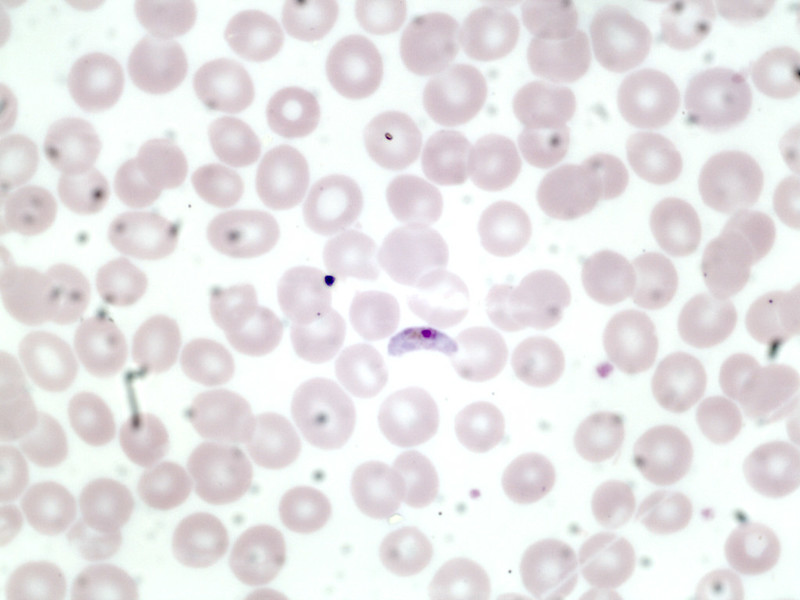
Ring Form (Early Trophozoite)
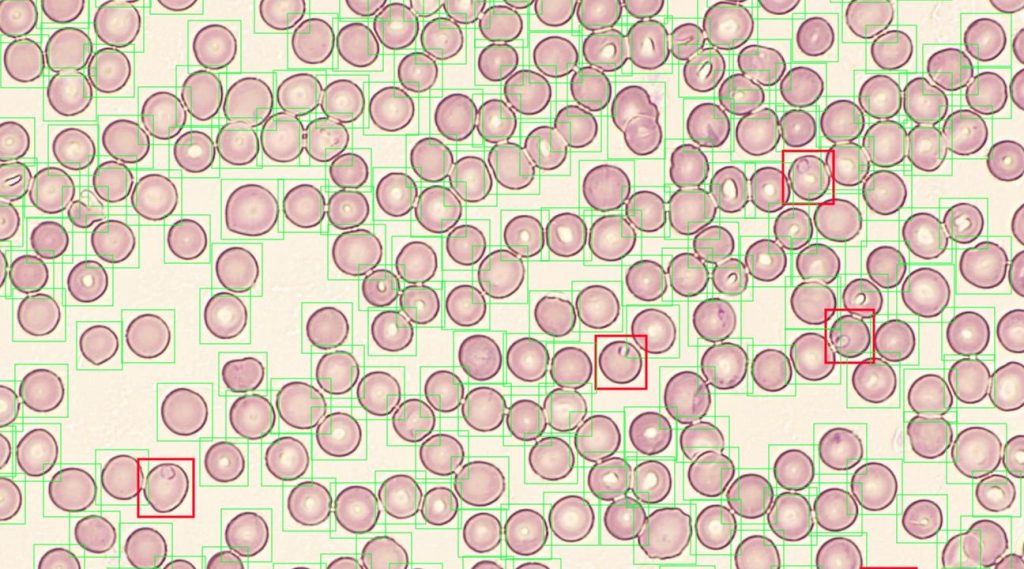
Source: NOUL
This is the first visible stage of the Plasmodium falciparum in a blood smear. The parasite is contained inside red blood cells (RBC), appearing as a thin blue ring (the parasite’s cytoplasm) with a tiny red dot (its nucleus) under the microscope.
Known as the falciparum ring form, it’s not uncommon to see multiple ring forms in a single RBC—a hallmark of P. falciparum. Other times, the ring seems to be stuck to the edge of the RBC, which is called an accolé or marginal form.
Trophozoite (Late Stage)
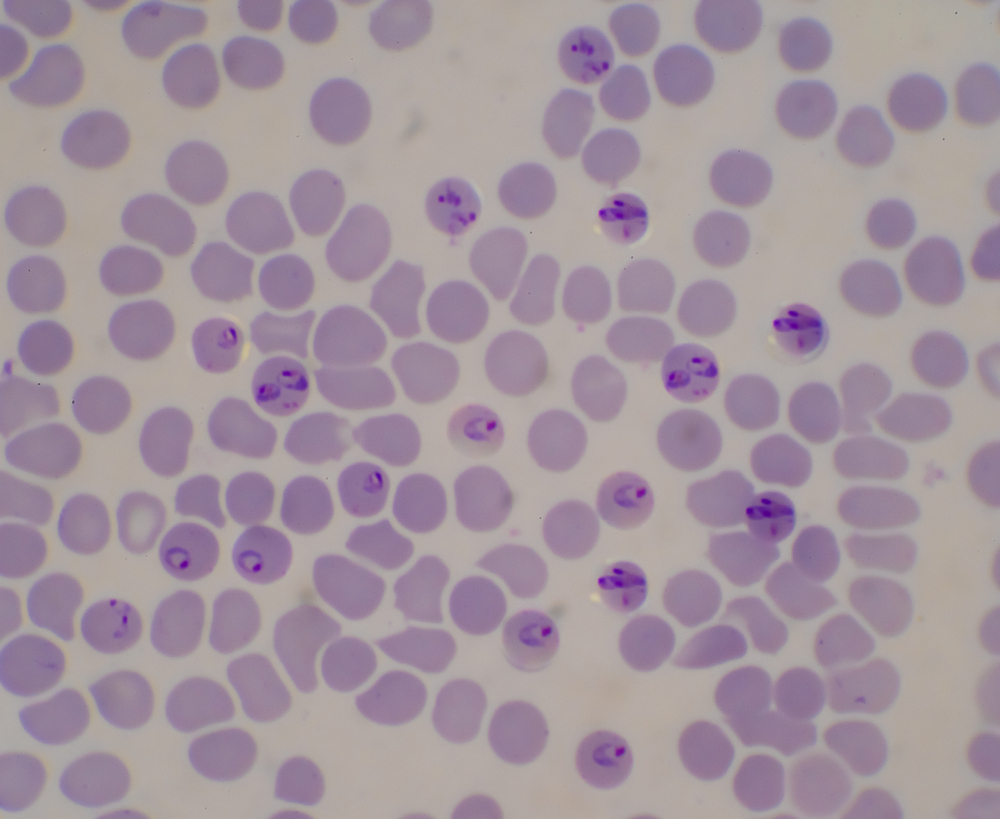
Source: Shutterstock
Trophozoites represent the active feeding stage of the parasite. Inside the RBC, it starts to grow and metabolize—it’s not extremely visible as the cytoplasm thickens and becomes more voluminous. You may also see hemozoin, a dark pigment produced when the parasite digests hemoglobin.
Schizont
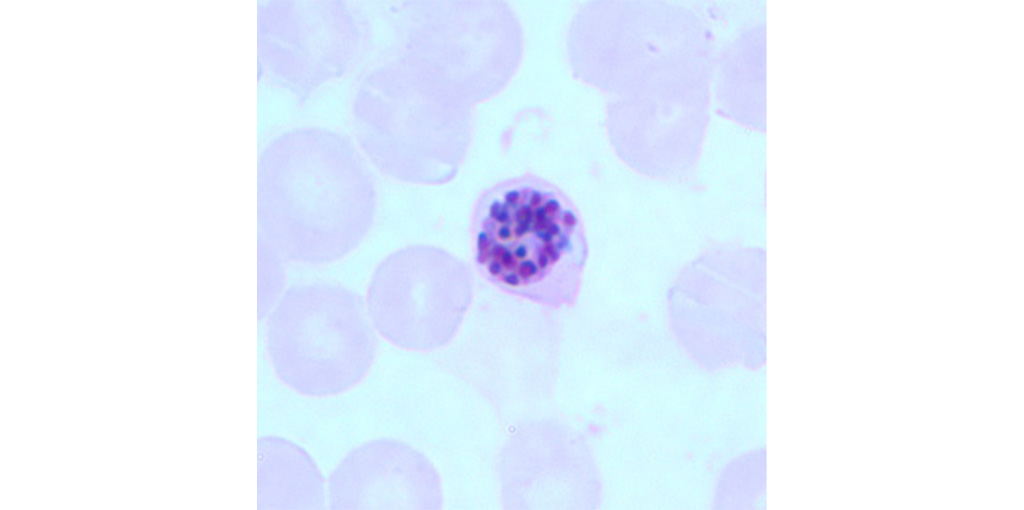
Source: CDC
The schizont is the self-replication phase (asexual reproduction). While still inside the RBC, the schizont divides into 8-24 merozoites, tiny daughter parasites. The RBC burst open, releasing the merozoites into the bloodstream.
Usually, schizonts aren’t visible under light microscopy as they hide in small blood vessels (capillaries)—a process called sequestration. However, if schizonts are visible in peripheral blood, it indicates very high parasite levels and severe malaria.
Gametocyte
Source: Flickr
The final relevant form of Plasmodium falciparum in blood smears is the gametocyte—the sexual stage of the parasite. It occurs around 10-12 days after infection (even if the patient is starting to feel better) and is marked by the gametocytes, which have a distinctive crescent or banana shape. Gametocytes are the transmissible form of the parasite, picked up by mosquitoes during a blood meal, beginning the life cycle all over again.
State-by-Stage Summary
Accurate identification of Plasmodium falciparum stages — including ring forms, trophozoites, schizonts, and gametocytes — is essential for reliable diagnosis and disease monitoring. Thankfully, each stage of the parasite’s lifecycle has a distinct clue: ring forms mark early presence, trophozoites reflect active growth, schizonts indicate high parasite loads, and gametocytes signal transmission potential.
In endemic regions, microscopy remains the only viable diagnostic method. However, due to infrastructural constraints, administration of timely and targeted treatment isn’t always possible. But, with better tools and training, we can boost diagnostic accuracy, relieving the malarial burden where it falls hardest.
Enhance Malaria Diagnosis with NOUL’s miLab™ MAL
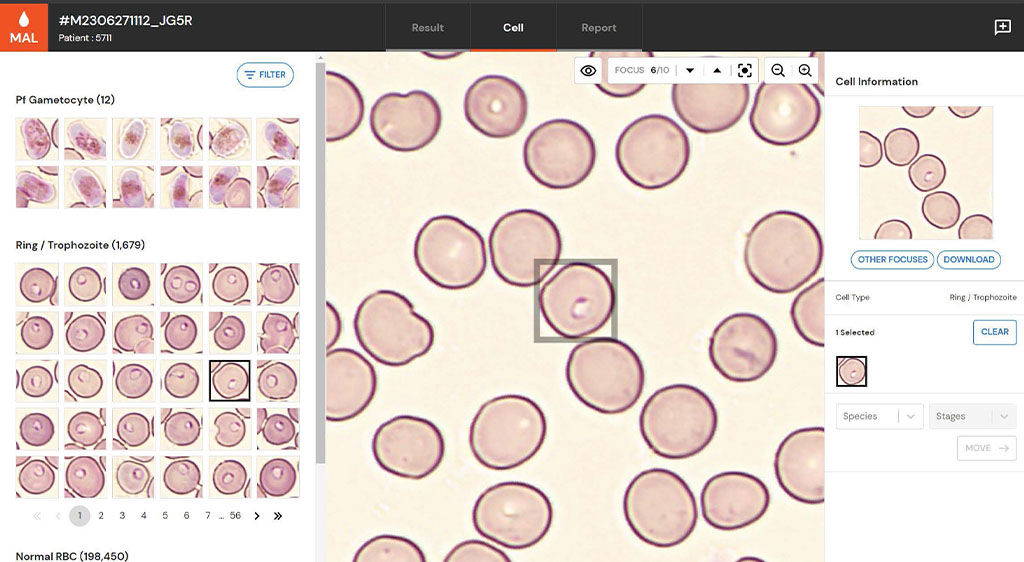
Source: NOUL
If only there were a diagnostic platform that could confirm a diagnosis of malaria in minutes without investing in expensive and difficult-to-maintain healthcare infrastructure. There is.
The miLab™ MAL by NOUL was specifically designed to help resource-deprived regions cope with malaria.
This next-generation AI-powered digital microscopy device automates and streamlines the diagnostic process. Using a patented technology—called Next-Generation Staining and Immunostaining (NGSI), it replaces the need for conventional liquid-based staining with a solid-state reagent system. So, no more expensive reagents and other supplies are needed.
The benefits? Well, the miLab™ MAL simplifies slide preparation, is portable, and has greater accuracy than its human counterparts. It’s perfect for use in challenging field environments such as rural clinics in Africa.
It even supports automated parasitemia level calculation, allowing users to include only early-stage parasites or all infected forms including gametocytes—tailored to clinical context.
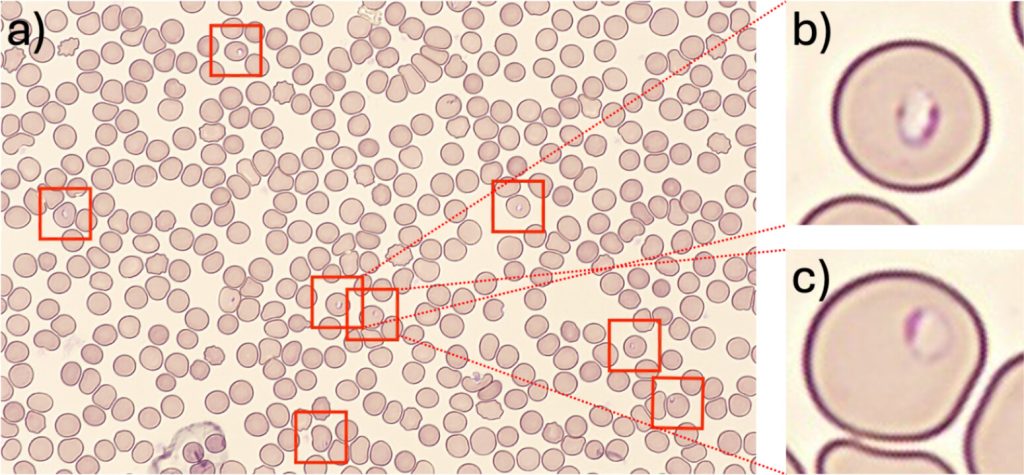
Source: PLOS
In fact, a recent peer-reviewed study of miLab™ MAL demonstrated outstanding diagnostic accuracy:
- Sensitivity: 94.3% for P. falciparum, 97.0% for P. vivax.
- Specificity: 94% for P. falciparum, 97.6% for P. vivax.
- Hrp2 Deletion Accuracy: Successfully diagnosed 98.1% of P. falciparum infections with hrp2/hrp3 gene deletions, which is crucial for overcoming the limitations of RDTs in such cases.
The miLab™ MAL isn’t just an impressive piece of technology—it’s a transformation tool for accurate, field-adapted malaria diagnosis. If deployed effectively, it can lead to earlier diagnoses and more successful treatment in some of the world’s most deprived regions.
Looking Ahead: World Malaria Day

Source: WHO
World Malaria Day 2025 takes place on April 25. It’s a chance to remind ourselves of the terrible burden of malaria globally and to push efforts towards malaria elimination.
This year’s theme, “Innovation for Impact: Diagnostics at the Frontline,” highlights the life-saving role of accessible, accurate, and field-adapted diagnostic tools in breaking the transmission cycle. As we continue to fight against malaria, new tools like the miLab™ MAL and further investment will protect vulnerable populations and save lives.
Ready to learn more or explore partnership opportunities? Get in touch with NOUL to talk about the miLab™ or understand its other applications. Partner with NOUL to transform malaria diagnosis.