Malaria continues to pose a global health challenge, with an estimated 249 million cases and 608,000 deaths across 85 countries in 2022, according to the latest World Malaria Report. This life-threatening condition is a drain on resources in developing countries, placing extreme pressure on healthcare systems in vulnerable, high-transmission regions.
Understanding how malaria is transmitted can provide insight into how to tackle the disease in the long term. Currently, Africa is the worst affected region worldwide, home to 94% of malaria cases and 98% of malaria deaths. Here, the Anopheles mosquito is the primary vector and the subject of substantial malaria prevention research.
In this article, we cover how malaria is transmitted, where it’s most prevalent, effective prevention strategies, and the value of high-quality diagnostics.
How Malaria is Transmitted
 Source : Freepik
Source : Freepik
The Role of Anopheles Mosquitos in Malaria Transmission
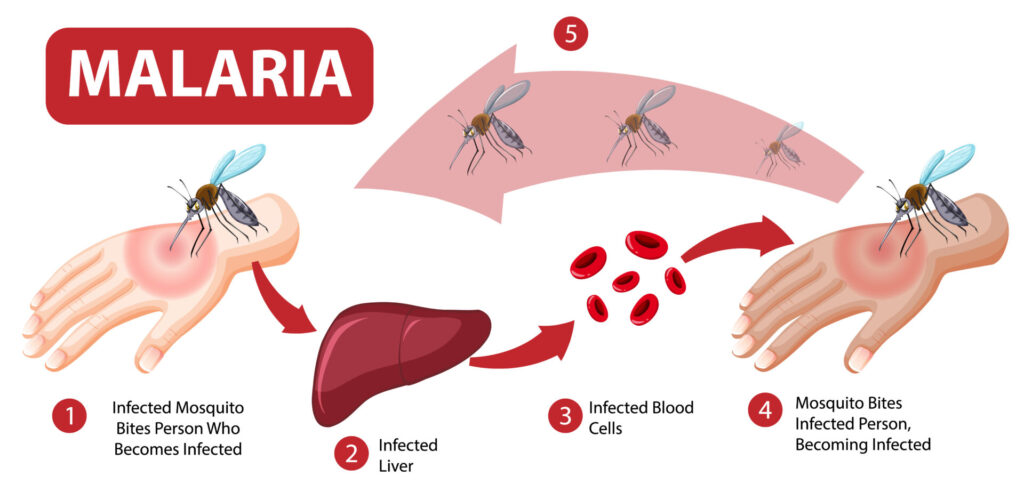
Malaria is caused by blood parasites of the genus Plasmodium. These parasites infect humans via the Anopheles mosquito, which act as the primary vector. After a human is infected and the parasite has been through its lifecycle, future mosquitos which bite an infected person will also become infected, thus beginning the lifecycle again.
Anopheles mosquitos are most common in sub-Saharan Africa and other warm, tropical and subtropical regions. The environmental conditions in these regions allow the parasite to multiply within the vector.
Lifecycle of the Plasmodium Parasite
Plasmodium‘s lifecycle involves three stages:
- Mosquito stage: The parasite develops from a gametocyte into an oocyst, releasing sporozoites. These sporozoites are injected into humans during a mosquito’s blood meal.
- Liver stage: Sporozoites infect liver cells, maturing into schizonts that release merozoites into the bloodstream.
- Blood stage: Merozoites infect red blood cells, completing their cycle and forming gametocytes, which can infect new mosquitos.
Different species of Plasmodium behave slightly differently. For example, P. vivax can spend months or several years dormant in the liver cells, reproducing asexually and causing persistent symptoms (known as relapsing malaria). In contrast, P. falciparum is more efficient in transmitting via mosquitos due to its higher parasitemia levels and shorter extrinsic incubation period in the mosquito host.
Human-to-Mosquito and Mosquito-to-Human Transmission Cycle
Humans serve as the reservoir for the parasite. Mosquito populations fluctuate based on seasonal changes, temperature, and the availability of standing water, which serves as breeding sites for Anopheles mosquitos. In the absence of mosquitos, the parasite persists in human liver and blood, allowing the disease to lay dormant for a while.
Regional Focus: Endemic Regions of Malaria
 Source : gettyimages
Source : gettyimages
Sub-Saharan Africa as a High-Risk Area
Sub-Saharan Africa has the highest rates of malaria infection worldwide. Several factors drive these rates, including tropical climates, high mosquito density, and socio-economic challenges that limit effective malaria control measures.
The primary parasite in Africa is the P. falciparum, which causes the most severe cases of malaria. That’s why it’s also the deadliest of the endemic regions of malaria. In 2022, Ethiopia, Nigeria, and Uganda reported significant case numbers, with Nigeria alone accounting for 27% of global malaria cases. Accurate and updated statistics from the World Malaria Report underscore the urgent need for intensified interventions in these high-burden countries. However, other nations like the DRC, Cameroon, Ghana, and Niger bear the brunt of infections.
Malaria in Other Endemic Regions
Malaria isn’t just an African problem. Regions such as Southeast Asia and South America also host significant outbreaks of the parasite. Home to dense rainforests, these regions have lots of standing water where mosquitos can reproduce.
Another growing problem is the introduction of invasive species. Mosquitos from one part of the world are now present in other regions due to increased mobility and tourism. This spreads malaria to regions that were previously unaffected by the disease.
Emerging Concerns in the EU Region
The European Union (EU) is increasingly concerned about the rise of malaria. Climate change is increasing the temperature in parts of the continent, creating favorable conditions for mosquito breeding.
Previously, Europe eradicated malaria through insecticide spraying, swamp draining, and drug therapy. However, recent travel, migration, and global warming are reintroducing the species to the Mediterranean basin. This new outbreak has the potential to overwhelm an EU healthcare system primarily set up for chronic, not infectious, diseases.
Transmission Prevention Strategies
 Source : Freepik
Source : Freepik
Vector Control Measures
One of the most effective strategies to combat malaria is to tackle the Anopheles mosquito. Insecticide-treated bed nets simultaneously prevent infection and kill the mosquito during the night. Indoor residual spraying (IRS), meanwhile, applies long-lasting insecticides to the walls and ceiling of homes where mosquitos are likely to rest after feeding.
These measures reduce human exposure to infected mosquitos by killing or repelling them upon contact with treated surfaces.
Other strategies involve larvicide (targeting infected mosquito breeding sites) or sterile insect technique (SIT), an emerging strategy that releases sterilized male mosquitos to reduce reproduction rates.
Preventive Medications and Vaccines
Anyone who has traveled to one of the endemic regions of malaria will have taken prophylactic medication. Examples include atovaquone-proguanil, doxycycline, and mefloquine. These medications prevent Plasmodium parasites from developing in the liver or bloodstream.
Recently, the RTS,S/AS01 malaria vaccine, the first WHO-recommended vaccine for malaria, has shown potential to reduce malaria rates by approximately 30-40% in young children living in endemic regions.
Community and Healthcare System Efforts
Many communities in endemic regions of malaria remain unaware of mosquito-borne risks. Raising public awareness is a key objective of initiatives by WHO’s Global Malaria Programme and NGOs like the Malaria Consortium. Their initiatives include distributing educational materials, promoting the use of insecticide-treated bed nets (ITNs), and training local health workers to educate and assist their communities. These organizations also monitor case numbers, deliver healthcare services in underserved areas, and implement vaccination campaigns to curb malaria transmission.
Early diagnosis of an outbreak is crucial to timely interventions. It can help control outbreaks, monitor which regions are affected, and save lives through medical treatment.
Introducing NOUL’s miLab™ – An Accurate Malaria Diagnostic Solution
 Source : NOUL
Source : NOUL
NOUL is a leader in advanced diagnostic solutions, developing new technologies for malaria detection. Reliable diagnostics help break the transmission cycle, alleviating the healthcare burden on endemic regions like sub-Saharan Africa.
The miLab™ MAL is an innovative diagnostic device that analyzes blood samples for malaria using AI-driven techniques. It provides rapid and highly accurate diagnoses, surpassing traditional methods such as microscopy and rapid diagnostic tests (RDTs). Its automated, portable design makes it an ideal solution for resource-limited settings, particularly in remote and underserved regions of developing countries.
With malaria a continuing burden globally, the miLab™ MAL presents a possible solution. It can help strengthen your malaria control efforts. Consider partnering with NOUL to upgrade your systems and support vulnerable people in endemic regions. Only through continued innovation in diagnostics can we combat malaria and guarantee global health security.