White blood cells (WBCs) are your body’s main defense against foreign pathogens. When an infection strikes, WBC numbers swell to counter the invasion. However, changes in WBC count and appearance can also signal a wide range of other conditions, including blood disorders and immune system dysfunctions.
Under a microscope, the morphology of WBCs—their size, shape, and internal structure—can provide important diagnostic clues. Features such as hypersegmentation or toxic granulation may indicate underlying health issues and help clinicians detect diseases early, before complications arise. WBC morphology can also reflect how effectively the immune system responds to infections and other medical challenges.
Let’s take a closer look at WBC changes:
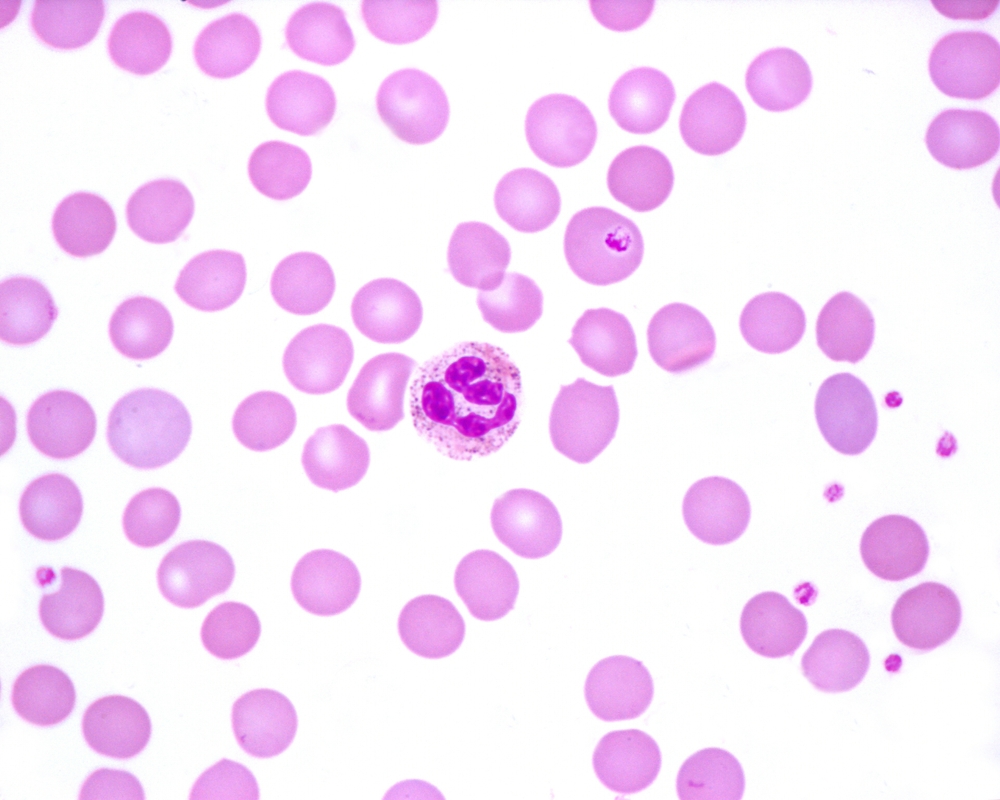
Toxic Granulation: Understanding the Key Features
Source: Shutterstock
Toxic granulation is defined as the presence of abnormal, large, dark-staining granules in the cytoplasm of neutrophils. These WBCs are the most abundant type, making up 50% to 80% of all WBCs. They’re crucial for fighting bacteria and viruses, and are spread throughout the blood, tissues, and lymph nodes.
The presence of toxic granulation in neutrophils often occurs due to infections, inflammation, or certain medications. It’s a clear sign of an active immune response—usually indicative of a bacterial infection or inflammatory condition. The granules are primarily composed of peroxidase and acid hydrolase enzymes.
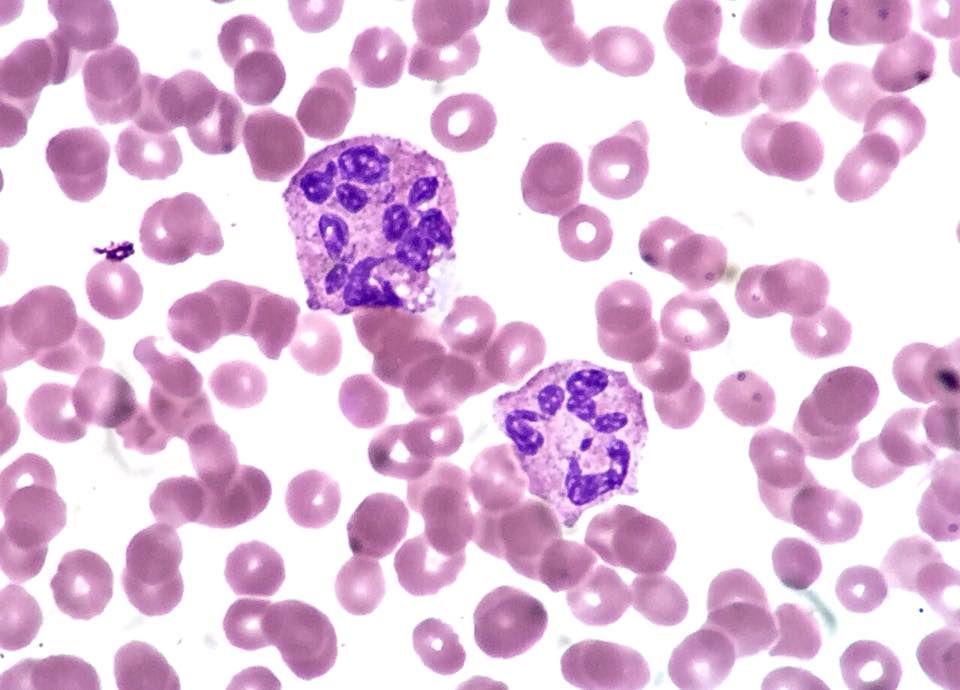
Hypersegmentation: What Does It Indicate?
Source: WikiCommons
Neutrophil hypersegmentation is another classic case of abnormal WBC morphology. It’s characterized as the presence of nuclei with six or more lobes or the presence of more than 3% of neutrophils with at least five nuclear lobes.
Hypersegmented nuclei are extremely easy to spot under a microscope. Usually, neutrophils have around three nuclear segments (lobes) connected by chromatin strands.
This change is linked to megaloblastic anemias, mainly caused by hypervitaminosis—either a vitamin B12 or folate deficiency. Other causes include myelodysplastic syndrome (MDS), myeloproliferative disorders, chronic infections, and chemotherapy/cytotoxic drugs.
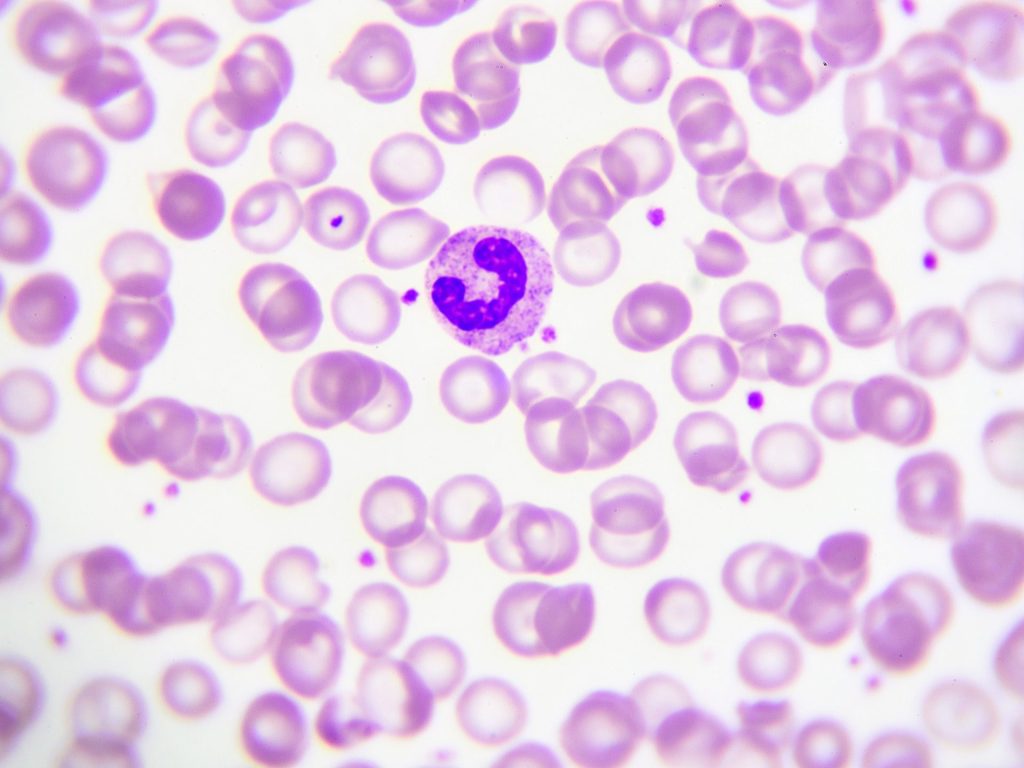
Banded Neutrophils: Immature Neutrophils in Action
Source: Shutterstock
Banded neutrophils, also known as band cells or stab cells, are immature granulocytes that are the precursors to neutrophils. These cells are identified by their curved, non-lobular nucleus, giving them a characteristic banded appearance.
These cells usually appear during an acute infection or stress response, when the demand for WBCs outstrips supply, triggering the release of immature neutrophils. This is known as bandemia or a “left-shift process” (an increase in the number of immature cell types).
Other forms of band cells occur for other granulocytes, e.g., basophils and eosinophils. However, the band is normally much more evident in neutrophils.
Pelger-Huet Anomaly: A Genetic Condition Affecting Neutrophils
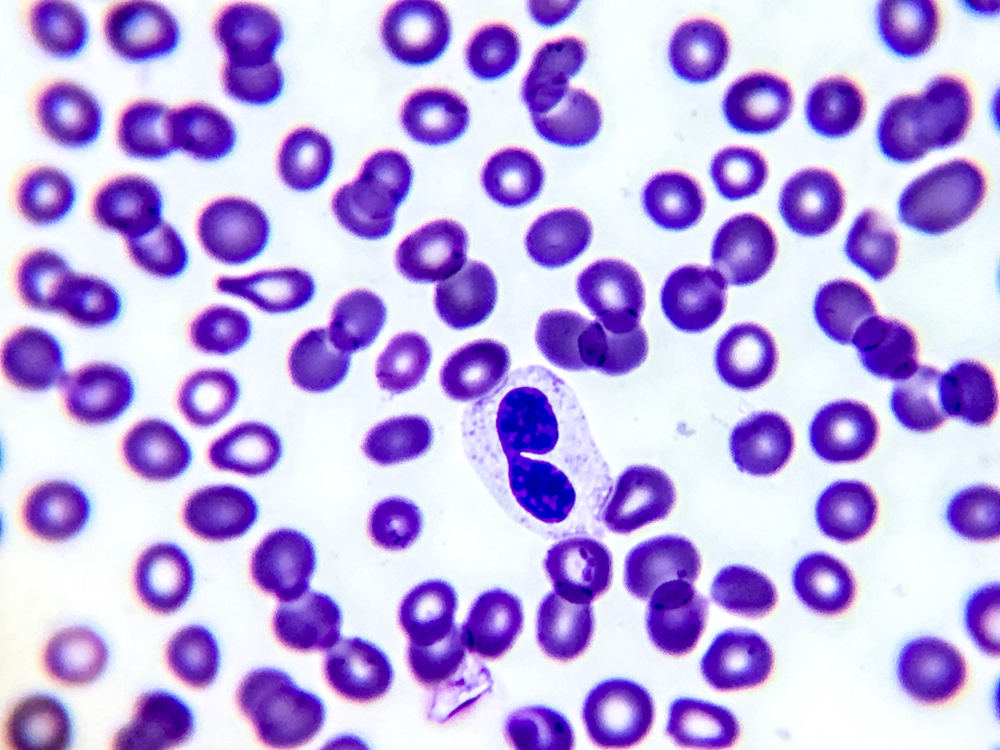
Source: Shutterstock
Unlike the other examples of abnormal WBC morphology, Pelger-Huet Anomaly is a genetic condition. This autosomal dominant genetic disorder is associated with neutrophils (and eosinophils) that have an unusually shaped nucleus. Characteristically, it is hyposegmented—being bilobed, peanut-shaped, or dumbbell-shaped.
The condition is classified as a blood laminopathy—associated with a mutation in the lamin B receptor, which plays a key role in nuclear structure and chromatin organization.
People with Pelger-Huet Anomaly will not experience any symptoms. The condition is typically picked up incidentally during a blood smear. However, it is important not to confuse the condition with myelodysplastic syndromes or infection.
An acquired version (pseudo-Pelger-Huet Anomaly) can occur due to myelodysplastic syndromes, leukemia, or drug toxicity.
The Importance of WBC Morphology in Diagnosing Health Conditions
When a person has any kind of health problem, a complete blood count (CBC) is the standard first-line diagnostic test. It gives an insight into the numbers of each of the blood cells. If a person’s WBCs are raised, it usually indicates an infection, inflammation, or a blood disease. In contrast, if they’re low, it could be a sign of a bone marrow disorder, autoimmune disease, nutritional deficiency, or medication.
WBC morphology goes beyond simple cell counts. It analyzes the shape, nuclear structure, and cytoplasmic features of WBCs (primarily neutrophils) to determine the underlying issue. That could be an acute infection, chronic inflammation, hematologic malignancies, or nutritional deficiencies.
Indeed, the WBC morphology provides context for the cell count. It doesn’t just say how many of each cell type are present but how they’re functioning and reacting to the disease. The result? A greater level of insight and understanding into the disease process, allowing more precise and early diagnoses.
However, WBC morphology isn’t assessed in isolation; when paired with a CBC, it provides a more comprehensive picture that guides clinicians toward effective treatment.
Enabling Effective Detection and Actionable Diagnosis with miLab™ BCM
Source: NOUL
How do we analyze WBC morphology? The answer is a blood smear. A small sample of blood is laboriously spread on a slide, dyed, and prepared for microscopic analysis. This takes time, resources, and expert insights to yield results—not available in resource-deprived regions.
The miLab™ BCM by NOUL performs the same action in a matter of minutes. Combining a CBC and morphological analysis into a single compact system streamlines workflows, eliminating the need for multiple instruments or expensive labs.
Powered by AI, the platform delivers both quantitative and qualitative insights into blood cell health. Clinicians can insert a blood sample and rapidly diagnose immune-related or hematologic conditions. Its innovative Next-Generation Staining and Immunostaining (NGSI), a novel hydrogel-based method developed by NOUL, requires neither liquid nor costly reagents, making it an eco-friendly, fully automated solution optimized for high-throughput testing.
Ideal for decentralized, remote, or under-resourced regions, the miLab™ BCM ensures consistent, accurate results while minimizing human error and reducing reliance on trained personnel. Highly portable and user-friendly, it’s useful for point-of-care (POC) use, making advanced diagnostics accessible even in the most challenging environments.
Ready to learn more about the miLab™ BCM? Explore our product page or contact us directly for a personalized demonstration of how the platform works in action. Transform your diagnostic workflow and embrace the future of medical testing.