When you receive a positive diagnosis, it’s confirmation that you have a condition. Whether your hemoglobin levels are low or you’ve got cancer cells in a biopsy, we trust medical tests to provide accurate, reliable information. Except: diagnostic accuracy is almost never 100%.
Diagnostic accuracy is a marker of how reliable a test is. It’s covered by several factors, including sensitivity and specificity, positive predictive value (PPV), and negative predictive value (NPV). Together, these factors determine the likelihood that a result is correct.
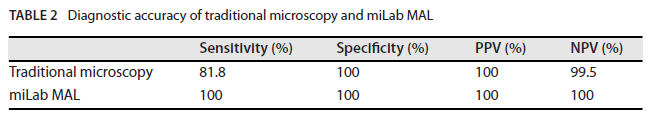
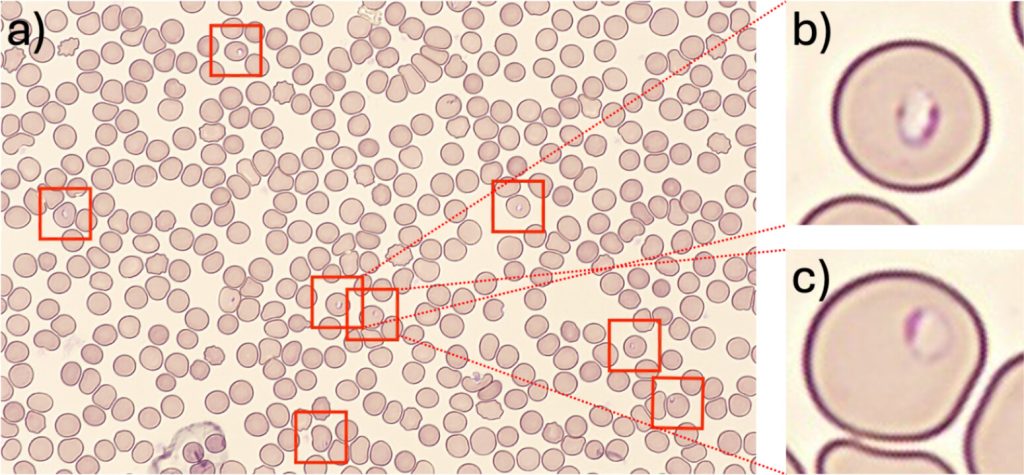
Source: Journal of Clinical Microbiology
NOUL works exceptionally hard to make our AI-powered diagnostic solutions as accurate as possible. In fact, in a reference lab study, miLab™ MAL showed 100% sensitivity, specificity, PPV, and NPV for detecting Plasmodium falciparum, matching the results of standard microscopy. What does this mean? And how does it affect clinical practice? Let’s find out.
What is Diagnostic Accuracy?

Source: Shutterstock
Diagnostic accuracy is simply defined as: “The ability of a test to correctly identify those with and without a disease.” We can think of this in two parts: (1) how likely a patient with a negative result is to have the disease and (2) how likely a patient with a positive result is to have the disease. We use sensitivity, specificity, PPV, and NPV to understand these questions.
Why does it matter? Well, doctors rely on test results to diagnose and treat patients. If the results aren’t accurate, a patient may receive an incorrect treatment or no treatment at all – increasing costs and harming patients. Several issues affect diagnostic accuracy, including sample quality and handling, variability in disease prevalence, and human and technical errors in interpretation.
Sensitivity vs. Specificity
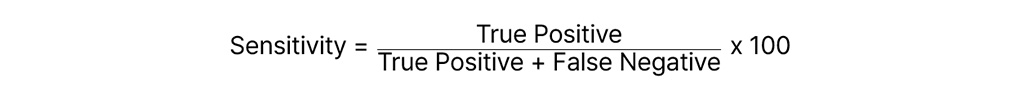
Sensitivity is a measure of the true positive rate. It describes the proportion of people with a positive test result who have the disease. The higher the sensitivity, the fewer false negatives occur. High sensitivity rates are crucial for tests where a missed diagnosis could be dangerous, e.g., cancer. For example, in a malaria test, a high sensitivity means most infected people are correctly diagnosed.
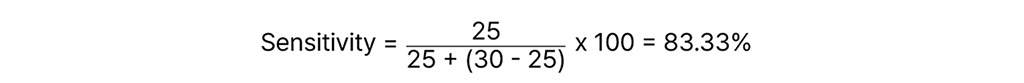
It’s a simple calculation:
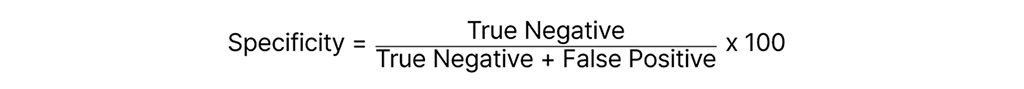
Specificity, on the other hand, is a measure of the true negative rate. It describes the proportion of people with a negative result who actually do not have the disease. The higher the specificity, the fewer false positives occur. It is incredibly important for preventing overdiagnosis and unnecessary treatments. For example, when screening for rare diseases, high specificity ensures healthy individuals are not wrongly diagnosed.
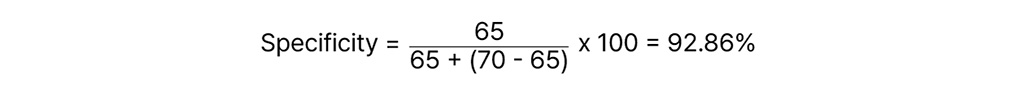
The calculation is:
No test is perfect – they’re always a trade-off between sensitivity and specificity. Doctors balance the risks of over- and underdiagnosis, selecting specific tests for different clinical scenarios.
How to Calculate Sensitivity and Specificity
Calculating Sensitivity
Suppose a new diagnostic test for detecting a virus is evaluated in a study involving 100 individuals. Out of these, 30 are known to be infected with the virus (true cases). The test correctly identifies 25 of these infected individuals as positive. Sensitivity measures the test’s ability to correctly identify those with the disease. Let’s put the numbers into the equation:
Calculating Specificity
In the same study, 70 individuals do not have the virus. The test correctly identifies 65 of these non-infected individuals as negative. Specificity measures the test’s ability to correctly identify those without the disease. Let’s put the numbers into the equation:
Common Errors to Avoid
It’s crucial to understand that test results vary between different populations. Factors such as age, gender, genetics, and preexisting health conditions can influence the accuracy of tests. Such population variability must be accounted for.
Another error to avoid is the influence of disease prevalence on perceived test performance. In populations where a disease is common, even tests with moderate sensitivity and specificity can appear highly effective due to the high number of true positive results. Conversely, in low-prevalence settings, the same test might produce more false positives, leading to an overestimation of disease incidence.
Positive and Negative Predictive Value
Positive predictive value (PPV) is the probability that a person with a positive test result has the disease. The calculation is:
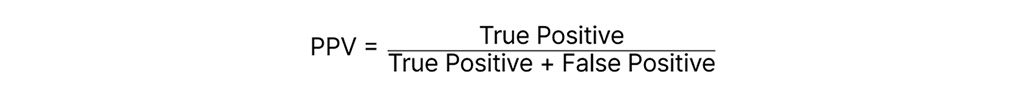
PPV is crucial for determining the reliability of a positive result. For example, prostate-specific antigen tests are raised in prostate cancer, but also several other conditions. The PPV for a PSA test, therefore, is low, undermining the reliability of the results.
Negative predictive value (NPV) is the probability that a person with a negative result does not have the disease. The calculation is:
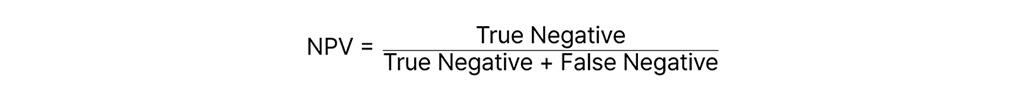
The higher the NPV, the more confidence a doctor has in the negative test results. This is critical for high-risk conditions like cancer, where a missed diagnosis can have dangerous consequences.
Several factors influence PPV and NPV, including disease prevalence (lower prevalence leads to lower PPV and higher NPV) and the overall population characteristics (sample selection bias).
Why Diagnostic Accuracy Matters for Healthcare Providers
Never underestimate the importance of diagnostic accuracy. If a test cannot be trusted, if a doctor cannot act on the results, then the test results aren’t useful.
Let’s consider some of the factors:
- Impact on Patient Care. Accurate, reliable test results are pivotal to timely and appropriate patient care. This minimizes the risk of misdiagnoses and unnecessary interventions.
- Operational and Economic Benefits. The more inaccurate a test, the more resources are wasted on unnecessary treatments. Worse, patients with a false negative will present later, requiring more costly interventions.
- Importance in Different Medical Fields. As mentioned, different scenarios require a preference for either high sensitivity or specificity. For example, infectious diseases (e.g., malaria) require a high sensitivity, so no cases are missed, whereas chronic conditions (e.g., diabetes) require a high specificity, so nobody is given a treatment they don’t need.
Source: NOUL
Newer technologies are pushing the boundaries of diagnostic accuracy. In a reference laboratory study, NOUL’s miLab™ MAL achieved 100% sensitivity, specificity, PPV, and NPV in detecting Plasmodium falciparum, matching standard microscopy and identifying additional positives initially missed. By leveraging AI-powered image analysis, miLab™ MAL minimizes human error and supports faster, more reliable diagnostic decisions for both patients and clinicians.
Conclusion

Source: NOUL
To sum it all up, diagnostic accuracy, which encompasses sensitivity, specificity, PPV, and NPV, is the cornerstone of effective medical testing. NOUL’s miLab™ MAL is revolutionizing this field with a stellar 100% in all these metrics. This AI-driven tool isn’t just about numbers—it’s about real-world impact, ensuring that patients receive the most accurate diagnoses possible, quickly and efficiently.
NOUL continues to engage with global experts to advance diagnostic science. Most recently, we joined the Scientific Spring Meeting of the Dutch Society of Medical Microbiology (NVMM) and the Royal Dutch Society of Microbiology (KNVM) 2025 in the Netherlands to share insights on AI-powered diagnostics and connect with leaders in microbiology and infectious diseases.
For healthcare professionals, adopting NOUL’s miLab™ means setting a new standard in diagnostic excellence and patient care. It’s time to step into the future of diagnostics, where accuracy meets technology. Get in touch today to learn more.