Introduction
Malaria remains a significant global health challenge, affecting millions annually, particularly in resource-limited regions. Accurate and efficient malaria diagnosis is critical to reducing mortality and improving morbidity.
Traditional and modern diagnostic tools, such as microscopic examination, rapid diagnostic tests (RDTs), and molecular diagnosis (PCR), provide unique features. The integration of these tools into a unified diagnostic framework can optimize detection and treatment strategies in diverse healthcare settings.
Microscopic Examination
Microscopy has long been considered the gold standard in malaria diagnosis. This technique relies on thick and thin blood smears to detect malaria parasites.
 Source : unsplash
Source : unsplash
Principle
Microscopic examination involves the preparation and staining of blood samples, which makes it possible for trained personnel to observe and identify malaria parasites under a microscope. Thick smears are used to detect the presence of parasites, whereas thin smears allow us to identify the type of species that are involved.
Advantages
- Facilitates accurate malaria diagnosis by enabling clear identification of species and quantification of parasitemia.
- Cost-effective and widely used in well-resourced laboratories.
- Provides valuable information about parasite lifecycle stages, aiding in effective treatment planning.
Challenges
- Requires significant time and skilled personnel to accurately interpret the results.
- Limited accessibility in low-resource settings (where malaria is most prevalent).
- Dependence on high-quality reagents and equipment.
Learn more about these challenges in NOUL at ASTMH 2024.
Rapid Diagnostic Tests (RDTs)
RDTs provide a fast and portable solution for malaria diagnosis. These tests detect malaria antigens through dipstick or cassette-based formats.
 Source : flicker
Source : flicker
How They Work
RDTs use monoclonal antibodies to detect specific malaria antigens in a blood sample. The results appear as visible lines on the dipstick or cassette (similar to a pregnancy test) within 15-20 minutes.
Advantages
- RDTs require only a dipstick, making them ideal for point-of-care use.
- Minimal training is required for effective operation.
- Portable, requiring minimal training and no specialized equipment.
Limitations
- Lower sensitivity in cases of low parasitemia.
- Unable to differentiate between malaria species or quantify parasitemia.
- Variability in performance based on product quality and storage conditions.
- Prone to false positives, and performance may decline with improper storage conditions.
Additional insights can be found at How Malaria is Transmitted.
Molecular Diagnosis (PCR)
Molecular diagnosis that uses PCR is a highly sensitive method that detects malaria parasite DNA with exceptional specificity.
Polymerase chain reaction (PCR) amplifies parasite DNA from a blood sample. This method precisely identifies malaria species and detects drug-resistant strains.
 Source : pexels
Source : pexels
Advantages
- Identifies the species and detects drug-resistant mutations.
- Its high sensitivity makes it ideal for research, surveillance, and outbreak tracking.
- Provides very high specificity for mixed-species infections.
Limitations
- Requires advanced laboratory infrastructure and trained personnel.
- Results are not immediately available, which limits the use in acute clinical settings.
- Expensive equipment and reagents increase operational costs.
For detailed testing protocols, visit CDC: Malaria Diagnostic Tests.
This table compares the different types of malaria diagnostic methods:
miLab™ MAL (A Comprehensive Diagnostic Solution)
miLab™ MAL is the new player in town. It addresses the limitations of traditional diagnostic tools through the integration of advanced technology into a single device.
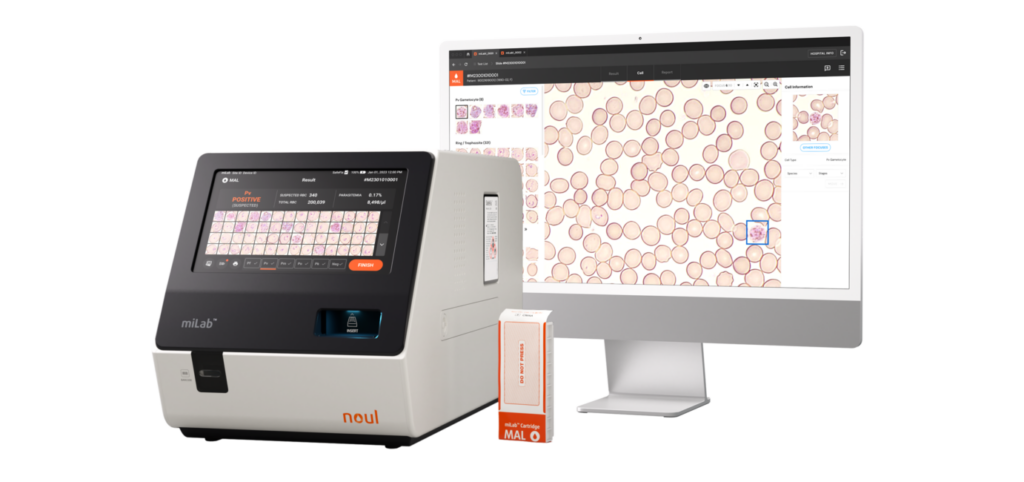 Source : NOUL
Source : NOUL
Capability
- Combines the precision of microscopic examination, the speed of RDTs, and automated workflows for a higher efficiency.
- Identifies species and quantifies parasites in a compact and portable device.
- Automates staining, imaging, and analysis, which reduces the risk of human error.
Accessibility and Versatility
- Suitable for both advanced laboratories and resource-limited settings.
- Eco-friendly design minimizes waste and operational costs.
- Its touchscreen interface and automated workflows simplify operation, even for minimally trained staff.
Learn more at Malaria Diagnostics Product.
How miLab™ MAL Impact Healthcare
The introduction of miLab™ MAL has the potential to transform malaria diagnostics around the world. Today, the challenges of resource variability are very important to address. In regions with high malaria burdens (e.g., sub-Saharan Africa, Southeast Asia), miLab™ MAL can significantly reduce diagnostic delays and improve disease management outcomes.
Collaborations with healthcare providers and government programs will further improve the device’s impact, which ensures that even remote communities benefit from its innovative features. Finally, its eco-friendly design aligns with global sustainability goals, which promotes the responsible use of resources in healthcare.
Conclusion
Microscopic Examination, RDTs, and molecular diagnosis (PCR) play indispensable roles in malaria diagnosis. However, they have some limitations:
- Microscopy – Remains the gold standard for species identification and parasitemia measurement but is time-intensive.
- RDTs – Fast and portable but less sensitive and unable to differentiate species.
- PCR – Highly sensitive but resource-intensive and unsuitable for acute cases.
miLab™ MAL revolutionizes malaria diagnosis through the integration of these methods, which provides a compact, accurate, and versatile solution that’s suitable for diverse healthcare environments.
Discover how miLab™ MAL can transform malaria diagnostics in your facility. Contact us today to learn more.